Overactive bladder
Incidence and causes
How often you pass water depends on several factors, but mainly on how much you drink. Most people pass urine fewer than eight times a day and not more than once during the night.
What is commonly known as “nervous bladder”, “irritable bladder” or “urgency incontinence” is referred to in medical terminology as “hyperactive or overactive bladder” based on the condition known as “overactive bladder syndrome”. An overactive bladder is common in men and women. 10-20% of all people are affected by it at some stage of their life and the incidence increases markedly with age.
Symptoms such as urgency or the need to urinate frequently are likely to have an adverse effect on a person’s quality of life. People suffering from symptoms of an overactive bladder often have to research the location of toilets before they leave home and run the risk of avoiding activities altogether. The lack of sleep caused by waking at night to pass water can additionally make it difficult to sustain daily activities because of the resulting tiredness. If urgency leads to loss of urine, it can cause embarrassing situations and affect self-esteem. These problems can also have an impact on family members. For instance, a partner may be woken up by night-time visits to the toilet. People avoid social activities because of their symptoms. This can also impact on the partner’s social life and lead to a feeling of isolation.
Symptoms of overactive bladder
The symptoms include:
- Sudden urge to urinate which is difficult to put off
- Any involuntary loss of urine
- The need to pass water more often than usual (more than 8 times in 24 hours)
- The need to wake up at night in order to urinate (=nycturia)
Diagnosis
As an overactive bladder is ultimately a diagnosis of exclusion, the doctor usually carries out various investigations before starting any treatment.
The most important thing is to take a detailed history so that the signs and symptoms are accurately recorded. Further investigations are often followed by urinary diagnostics to exclude a urinary infection, for example, as well as an ultrasound scan of the urinary system (bladder, kidneys, measurement of residual urine). For men palpation or ultrasound imaging of the prostate is additionally recommended.
It is often helpful to get affected patients to keep a urination diary. This records drinking habits, total number of visits to the toilet (passing water) during the day and at night, with a note of the volume of urine over several days. This provides a more objective picture of how many visits to the toilet the person has actually made and how severe the symptoms are. As treatment progresses, the diary can also be used as an objective measure of how successful it is.
Treatment options
Treatment takes place in stages and drug and non-drug options are available.
Non-drug therapy involving behavioural advice forms an important foundation for treating hyperactive bladder.
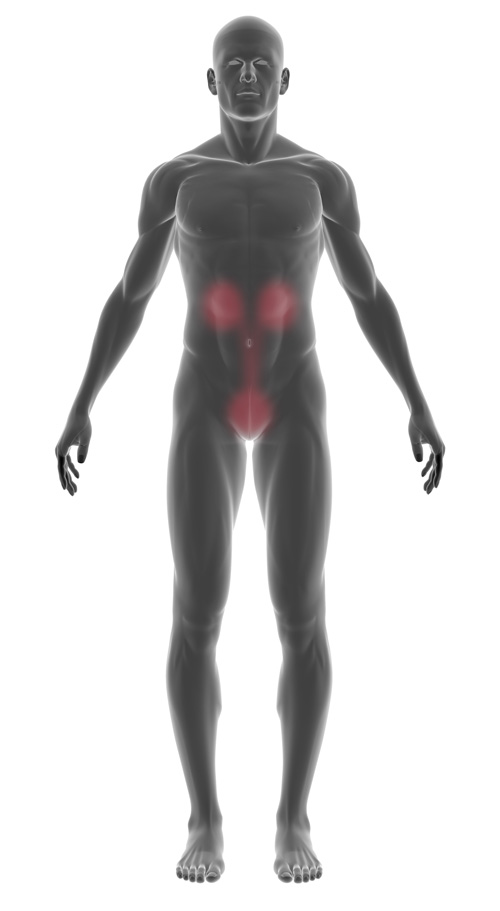
Pelvic floor exercises also help people with hyperactive bladder. However, behavioural changes are also very important, which include adjusting how much you drink.
Various classes of pharmaceutical are available to you for drug therapy:
- muscarinic receptor antagonists
- beta-3 agonists
- desmopressin
Muscarinic receptor antagonists are a group of pharmaceuticals that reduce abnormal contractions of the bladder and reduce the urge to urinate. They are the most commonly recommended group of drugs for the treatment of overactive bladder symptoms. The side effects of this drug are generally mild. They can include dry mouth, dry eyes, heartburn and constipation.
Beta-3 agonists are a new class of drug and have a different mechanism of action. They promote relaxation of the bladder during filling, increase bladder capacity and lengthen the interval between bladder emptying. The side effects are generally mild.
Desmopressin reduces the amount of urine the body produces. This drug is recommended if your major symptom of an overactive bladder is nycturia.